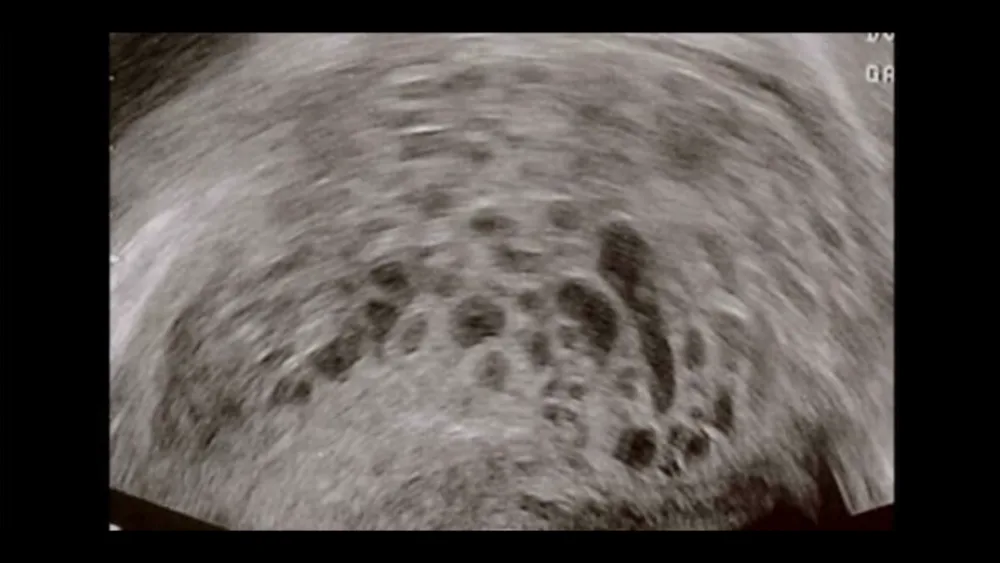
molar pregnancy (Hydatidiform Mole) is an incomplete pregnancy condition where the embryo and placenta do not develop properly. Instead, the tissue that would normally form the embryo becomes a non-cancerous tumor in the uterus. Normally, the placenta provides nutrients to the fetus and removes waste, but if the cells that form the placenta function abnormally after fertilization, it leads to the formation of cysts or fluid-filled sacs that resemble a cluster of grapes or fish eggs. These abnormal cells rapidly grow in the uterus instead of developing into a fetus, resulting in a molar pregnancy. While a molar pregnancy is a non-cancerous tumor, it is considered a precancerous condition, potentially leading to gestational trophoblastic disease or choriocarcinoma (a cancer of the placenta).
Symptoms of Molar Pregnancy
The symptoms of a molar pregnancy can resemble a normal pregnancy, but with some signs of a miscarriage mixed in, leading many women to mistakenly believe they are having a miscarriage. The symptoms of a molar pregnancy include:
-
Vaginal bleeding early in pregnancy: This typically starts around 4 weeks of pregnancy and the blood can range from dark brown to light red. Sometimes, tissue resembling grapes may be passed.
-
Sudden abdominal pain and an abnormally enlarged uterus: This causes cramping in the pelvic area and a swollen abdomen that is larger than expected for the gestational age, resembling a multiple pregnancy.
-
Severe nausea and vomiting.
-
Fatigue due to heavy vaginal bleeding.
-
Signs of hyperthyroidism: These include easy fatigue, a rapid heartbeat, excessive sweating, and pale skin.
-
Signs of preeclampsia: High blood pressure and the presence of protein in the urine.
Causes of Molar Pregnancy
The exact cause of a molar pregnancy is not yet fully understood, but it is more commonly seen in pregnant women who are either very young or over the age of 40, such as in teenage pregnancies or pregnancies in women over 40. The danger of a molar pregnancy is that it can develop into cancer. It is estimated that 1 in 5 molar pregnancies may turn into cancer. However, if treated early, the chances of a full recovery are 100%. If left untreated and allowed to progress, it becomes more difficult to treat.
A molar pregnancy is divided into two types:
A molar pregnancy without a fetus occurs when the fertilized egg contains only chromosomes from the father, resulting in the absence of an embryo, amniotic sac, or normal placental development. Instead, numerous cysts resembling a cluster of grapes grow in the uterus.
In a molar pregnancy with a fetus, the fertilized egg contains 23 chromosomes from the mother and 46 chromosomes from the father, leading to a total of 69 chromosomes. This condition arises from chromosome duplication from the father's side or from two sperm fertilizing a single egg. In most cases, the developing fetus is abnormal and cannot survive.
Risk Factors for Molar Pregnancy
Pregnant women who are under 18 years old or over 40 years old have a higher risk of a molar pregnancy. Women over 40 have a five-fold increased risk, possibly due to the higher likelihood of abnormal fertilization as women age. On the other hand, women under 18-20 years old have a slightly increased risk.
-
First-time pregnancy: Women who are pregnant for the first time may have a higher risk of a molar pregnancy.
-
History of molar pregnancy: Women who have had a molar pregnancy once have a 1-2% chance of having another molar pregnancy in the future. If they’ve had two previous molar pregnancies, the risk increases to 16-28% in subsequent pregnancies.
-
Nutritional factors: Studies have shown that low intake of carotene and vitamin A deficiency can increase the risk of a molar pregnancy without a fetus.
-
Irregular menstruation and contraceptive use: Women with irregular menstrual cycles or a history of using contraceptive pills are at an increased risk of a molar pregnancy with a fetus or fetal tissue present.
-
Smoking: Smoking is a risk factor for molar pregnancy.
-
Genetics: Family history or genetic factors may contribute to the risk of molar pregnancy.
Treatment for Molar Pregnancy
Pregnant women diagnosed with a molar pregnancy will not be able to continue their pregnancy and should receive treatment to prevent complications. The treatment options include:
-
D&C (Suction Curettage): This is the most common treatment method. It is both a diagnostic and therapeutic procedure that involves removing tissue for pathological examination.
-
Hysterectomy: This is considered for women over 40, who have a higher risk of cancer (2-3 times more likely), women with a large number of molar pregnancy cysts at high risk of cancer, women who no longer wish to have children, or women who experience severe bleeding from uterine rupture.
-
Prophylactic Chemotherapy: This may be used to prevent further complications.
-
Monitoring Hormone Levels: Regular monitoring of hormone levels is important after the treatment.
-
Contraception: Women are advised to use contraception during the hormone monitoring period, which typically lasts for about 1 year until the hCG levels normalize.
However, women who experience a molar pregnancy typically do not face issues with infertility or pregnancy-related health problems. They are also not at increased risk for fetal death, congenital disabilities, preterm birth, or other complications. The risk of a molar pregnancy occurring in future pregnancies is only 1-2%.
If you have any concerns, you can consult with Beyond IVF or contact us through Line @beyondivf for more information.






